Polypharmacy in Australia
Speaking to my mother, who lives in the US, over the phone last week, she was lamenting the number of medicines she takes each day. “I’m like a walking pharmacy,” she often jokes. Her list includes Metformin and Lantus (insulin glargine) for Type 2 diabetes, Escitalopram for low mood, Dexamethasone for Rheumatoid Arthritis, Rosuvastatin for cholesterol, Esomeprazole for reflux, Perindopril for high blood pressure, Methotrexate for lupus, Pregabalin for fibromyalgia. She has a few others as well, but these she doesn’t take every day. They are only “as needed”, she says.
The contents of my mother’s medicine cabinet never fail to spark a heated conversation between myself and my older sister. In essence, we question the necessity of each medication. We worry about her understanding of their purposes. We worry about possible harmful interactions. We worry about the frequent introduction of new medications by different specialists, creating a seemingly endless cycle of prescriptions.
This phenomenon is not unique to my family. Polypharmacy, the regular use of five or more prescribed medications, is a growing concern in Australia, particularly among the elderly. According to the Australian Bureau of Statistics, a staggering seven out of ten people aged 75 or over are taking at least five different medications. Overall, 18.9% of the Australian population are dispensed on average, 5 or more medication types. This trend highlights the urgent need for a more critical approach to medication management.
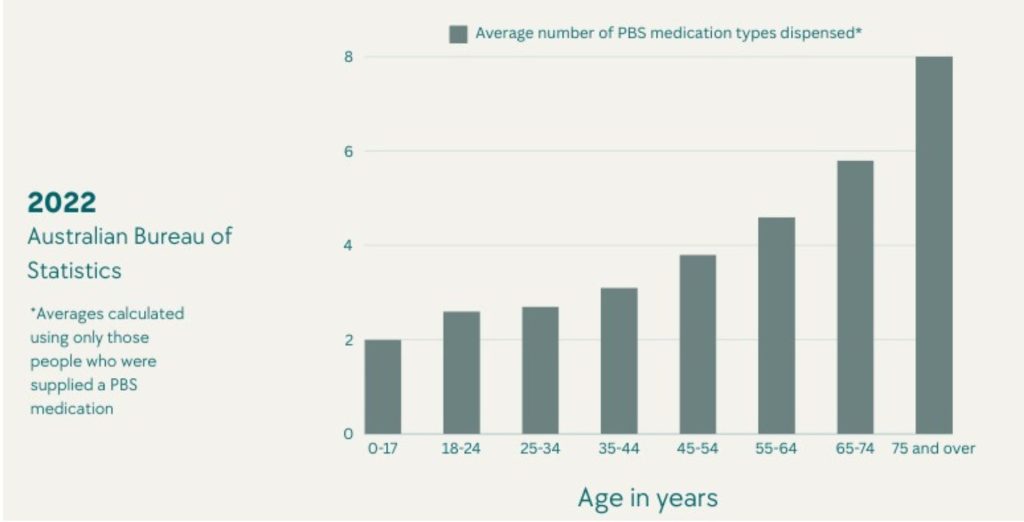
Figure 1. Average number of PBS medication types dispensed by age group in the 2022 census year. Medications, 2022 | Australian Bureau of Statistics (abs.gov.au)
Several factors contribute to the increasing prevalence of polypharmacy. One significant factor is the growing number of chronic conditions affecting the population. As people live longer, they are more likely to develop multiple health issues that require medication management. Additionally, the aging population is particularly vulnerable to polypharmacy due to physiological changes that can affect drug absorption, distribution, metabolism, and elimination.
The healthcare system itself can contribute to polypharmacy. The fragmented nature of Medicare, with multiple doctors and specialists diagnosing conditions and prescribing medications without adequate communication, can lead to overlapping or redundant treatments. Moreover, the pharmaceutical industry’s aggressive marketing of new drugs can influence prescribing practices, sometimes leading to unnecessary medication use.
The Risks of Polypharmacy
Research has shown that quality of medical treatment can be compromised when patients are taking multiple medications. As the number of drugs increases, so does the risk of adverse interactions, reducing treatment effectiveness and potentially causing harmful side effects. Some of the potential risks include:
- Complex Drug Interactions: Taking multiple medications can lead to intricate interactions between drugs. These interactions can amplify or diminish the effects of medications, potentially causing unintended side effects or reducing their therapeutic benefits. For instance, one drug might accelerate the breakdown of another, lessening its effectiveness, or two drugs might combine to create a harmful effect.
- Balancing Act of Medications: When patients have multiple health conditions, prescribing medications can be a delicate balancing act. A drug effective for one condition might inadvertently worsen another. For example, a medication for arthritis might elevate blood pressure, complicating the management of both conditions.
- Increased Risk with Multiple Medications: The more drugs a person takes, the higher the likelihood of experiencing adverse effects. This is particularly concerning for older adults, who are more susceptible to medication-related issues. Common side effects include confusion, dizziness, and falls, which can significantly impact quality of life and independence.
- Inappropriate Medications and Vulnerability: As the number of medications grows, so does the risk of taking unnecessary or even harmful drugs. Older adults are especially vulnerable to this, as their bodies often respond differently to medications compared to younger individuals. Benzodiazepines, frequently prescribed for anxiety and sleep, highlight this issue. While they can be beneficial in certain cases, their long-term use is often associated with increased fall risk, cognitive decline, and addiction.
- Unravelling the Impact of Polypharmacy: Polypharmacy has been linked to a range of health problems, including frailty, hospitalisations, and emergency room visits. However, pinpointing the exact contribution of polypharmacy to these issues is challenging due to the complexity of factors involved. Many individuals with polypharmacy also have multiple underlying health conditions, making it difficult to isolate the specific impact of their medications.
Dr Tonya Coren, Clinical Director for First Light Healthcare and Raindrum describes polypharmacy as a complex issue, largely due to the difficulty in predicting how different medication combinations will affect a patient’s health. “Taking multiple medications can be very tricky,” says Dr Coren, “It’s like juggling several balls at once. Each drug can interact with another, sometimes causing unexpected side effects. Plus, as you get older, your body processes medications differently, which can increase the risk of problems. That is why it’s important to regularly review your medications with your doctor to make sure they’re still necessary and working as intended,” she continues, “We want to balance the benefits of your treatment with the potential risks.”
The Medicalisation of Life: Are We Over-diagnosed?
Over the past decade, Australia has seen a steady increase in chronic disease diagnoses, particularly in mental health, according to 2022 ABS data. There’s a concerning trend of prescribing antidepressants to manage what were once seen as normal emotional responses—like sadness, loneliness, and grief—associated with different life stages.
ADHD is another condition that some argue is being over-diagnosed across all age groups in Australia. Behaviours such as inattention, disorganization, forgetfulness, lack of self-regulation, and impulsivity are increasingly attributed to ADHD. However, these behaviours exist across a wide spectrum of human experience and can occur at any stage of life. Yet, like many diseases, our healthcare system often focuses more on managing symptoms rather than addressing root causes.
The line between normal and abnormal is becoming increasingly blurred. Even small changes in diagnostic criteria can significantly increase the number of people diagnosed and prescribed medication. The threshold for many common conditions, such as high blood pressure or cholesterol, encompass a broad normal range of values. Treating borderline cases aggressively can lead to unnecessary medication, and, for some patients, harmful side effects that could have been avoided.
Deprescribing: A Path to Better Health
The term “deprescribing” can be described as a careful process involving systematically reviewing a patient’s medication regimen to identify treatments that are no longer necessary or where existing or potential harms outweigh potential benefits. While multiple medications are often justified, deprescribing optimises treatment by eliminating unnecessary drugs, reducing adverse reactions, and improving overall health.
Dr Coren compares the process of deprescribing to decluttering your medicine cabinet. “Sometimes less is more,” she says. ”By carefully reviewing your medications, we can often find those that aren’t needed anymore or aren’t working as well as we’d hoped.”
By reducing the number of medications taken, the likelihood of experiencing unwanted side effects diminishes significantly. These side effects can range from mild inconveniences to severe health complications. As an additional benefit, deprescribing can enhance a patient’s quality of life by alleviating the burden of managing multiple medications, improving adherence to necessary treatments, and potentially reducing healthcare costs.
While the concept of deprescribing is gaining traction, its implementation faces several significant challenges. One of the primary hurdles is overcoming the inertia associated with prescribing. Healthcare providers often feel pressured to offer treatments, and there can be a reluctance to discontinue medications due to concerns about potential adverse outcomes or patient dissatisfaction. Additionally, the complexity of polypharmacy, with multiple medications interacting in intricate ways, can make it difficult to determine which drugs to reduce or discontinue.
Another challenge lies in patient perceptions and expectations. Many patients have a strong belief in the necessity of their medications and may resist any attempts to reduce them. This can be particularly challenging for older adults who may have developed a strong trust in their healthcare providers and their prescribed treatment plans. Furthermore, the lack of clear guidelines and standardised protocols for deprescribing can hinder its implementation. There is a need for evidence-based frameworks to support healthcare providers in making informed decisions about medication reduction.
“Deprescribing can be a very proactive approach to medication management that prioritises patient safety and well-being,” says Dr Coren, “Too often, patients feel helpless and at the mercy of their medication. With the right management, individuals can be empowered to take control of their healthcare and work collaboratively with their healthcare providers to achieve the best health outcomes.”
The Importance of Medication Assessments
Regular medication assessments are crucial for preventing polypharmacy and its associated risks. These assessments should involve a comprehensive review of a patient’s medical history, current medications, and overall health status. By identifying unnecessary or potentially harmful drugs, healthcare providers can work with patients to develop tailored treatment plans.
It’s essential to foster open communication between patients and healthcare providers during these assessments. Patients should feel comfortable asking questions, expressing concerns, and actively participating in decision-making about their medication regimen.
If you’re concerned about your medication regimen or that of a loved one, here are some tips for discussing deprescribing with your doctor:
- Create a comprehensive medication list: Include the name, dosage, and reason for each medication.
- Be specific about your concerns: Clearly articulate your worries about the number of medications, potential side effects, or any other issues.
- Ask questions: Don’t hesitate to inquire about the purpose of each medication, potential alternatives, and the risks and benefits of reducing or stopping a particular drug.
- Consider a medication review: Request a comprehensive review of your medications to identify any that can be safely reduced or discontinued.
- Find a knowledgeable healthcare provider: Seek a doctor who is open to discussing deprescribing and has experience in medication management.
At Raindrum, medication management is a cornerstone of our programs. Our experienced medical team work closely with each client to optimise their medication regime, while actively exploring opportunities to reduce reliance on prescription medications. Aligned with the latest research, we believe that many chronic conditions can be effectively managed through dietary adjustments, exercise and other lifestyle modifications. Our approach is to prioritise supporting our clients in embracing positive lifestyle changes as the first step to achieving a healthier future.
Remember, you are your own best advocate. By taking an active role in your healthcare and having open conversations with your doctor, you can work together to optimise your medication regimen and improve your overall well-being.



